What is self-harm?
Self-harm involves intentionally causing injury to oneself, often as a manifestation of a psychological disturbance which is commonly triggered by an acute stressor or an interpersonal conflict. It is also called self-injurious behaviour or deliberate self-harm. It can take many forms including medication overdose or poisoning and wounding oneself via cutting, headbanging or burning.
Why does a child self-harm?
Self-harm in the majority of young people is in response to strong emotions which are often felt in the extremes for example anger and sadness. The physical act of self-harm can be a form of release which helps to stop a person feeling the overwhelming extremes of these emotions, providing some respite from the intensity of the emotions they are experiencing.
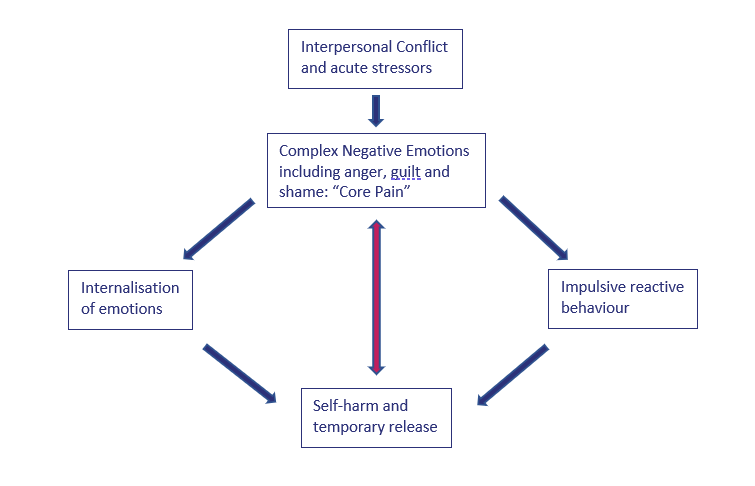
Self-harm is a complex behaviour pattern that is used when a child can’t regulate their emotions in alternative forms. The pattern of behaviour can be cyclical, with negative thoughts and behaviours perpetuating one another, as demonstrated below. With the correct support the cycle can be broken.
How common is self-harm?
Current data is likely to underestimate the community rates of self-harm but despite this, the prevalence of self-harm in children and adolescents has increased significantly in recent years. Data from the office for National Statistics shows that over the past two decades, rates of non-suicidal self-harm have increased across the whole population with some studies reporting that the rates of self-harm amongst younger children may have doubled in the past six years (between 2013 and 2020).
When should you refer to a specialist?
The way in which an individual self-harms can be stereotypical, following a specific pattern of behaviour but it can also evolve becoming more severe over time. It is important that specialist help is sought at the earliest opportunity as early intervention is key to prevent perpetuation and progression of the self-harming behaviour as well as aiming to resolve any other underlying social, psychological or interpersonal difficulties the child might be experiencing.
Who should you refer to?
The GP or the Special Educational Needs Co-ordinator (SENCO) or school nurse. If there are acute concerns regarding a child’s safety or wellbeing, it is recommended that a child attends the emergency department and receives specialist assessment from the child and adolescent mental health team in the hospital.
What options are available to manage self-harm?
There are a number of treatment options available which include at the core helping a child emotionally regulate in a more controlled manner. This can involve psychoeducation, talking therapy, identification of unhelpful thought patterns or stressors and in some cases identification and treatment of an underlying mental illness which may require further treatment with medication or alternative psychological interventions and social support.
Practical support strategies can help to prevent an individual acting on an impulse to self-harm acutely and these include:
Distraction
This can be personalised to the child; they might like to paint or draw or perhaps they might want to relax with a bath or a favourite film.
Exercise
Going for a walk in the playground or engaging in sports activities.number of women needing emergency accommodation.
Speak with others
A child might find it helpful to talk to someone they trust about the way they are feeling, perhaps a teacher or a parent.
Spend time with others
If a child does not want to talk with a trusted person, spending time with someone can be helpful.
Write in a journal
Some children might find it helpful to write their feelings down in a journal and might find this easier than talking to someone especially if they have difficulty expressing their emotions.
Controlled breathing
Sometimes focusing on the pattern and rate of breathing can help to distract from intense emotions. Try helping the child to breath in a slow and controlled manner with limited environmental distractions.
Less harmful alternatives
If none of the above are useful, less harmful physical expressions of emotions can be considered as alternatives e.g., holding an ice cube, squeezing a stress ball or hitting a pillow.

